Getting Started with State Coalitions and Associations
A few months ago, I received a phone call from someone regarding a bill that was moving through his state legislature.[1] This bill included language that palliative care should be made available to patients in a certain care setting—an accomplishment, he thought—but the description indicated that palliative care was only appropriate for patients nearing the end of life. The gentleman was new to advocacy, but he had already called several legislators, written letters, and was searching for opportunities to testify that the definition of palliative care needed to be moved further upstream. Despite his efforts, however, the bill was progressing rapidly without any modifications to the description of palliative care, and he wanted to know what else he could do. I happened to know that his state had an active hospice and palliative care organization, and asked what its approach had been to this legislation. His response was, “what is that organization?”
The National Coalition for Hospice and Palliative Care recently published its inaugural blog highlighting the importance of working collectively at the national level to address public policy challenges, improve communication, and share resources. One could argue that it is equally important to participate in this work locally, since much of your ability to provide high-quality care to patients with serious illness is linked to state policy. For instance, does your license allow you to provide non-hospice palliative care services? Is there a policy that could potentially limit your ability to prescribe opioids to patients in need? What must you do to ensure that your patient’s advance directive is followed?
Given the current administration’s ongoing commitment to shift risk and responsibility for health care payment to states, as well as states’ power to expand palliative care access, now is a great time to get involved. But a word of caution – do not try this alone! Promoting a policy or initiative can be complicated and resource-intensive and, while individuals can make enormous contributions, most of us are simply not as effective working independently as we are when working together.
Benefits of Participating in a State Palliative Care Coalition or Association
When it comes to state initiatives, there can be different opportunities for participation – coalitions, associations, organizations, task forces, councils, etc. Each will operate differently based on its mission, structure, stakeholder composition, and funding source. For the purpose of this blog, however, the phrase “state palliative care coalition or association” is intended to describe any state-based group that is working collectively to advance palliative care.
So what are some of the benefits of participating in a state palliative care coalition or association? The Robert Wood Johnson Foundation points to the fact that diverse stakeholder coalitions can maximize the use of resources, raise awareness of the issues, and help hard-to-reach populations. In the instance of the gentleman described above, participating in a coalition or association could have helped him be more strategic in his advocacy. If the proposed legislation was on the coalition or association’s policy agenda, it is likely that he would have had access to information on key stakeholders (e.g., legislators who serve on relevant committees) and clear messaging on the bill’s benefits and/or drawbacks that would resonate with those stakeholders. Furthermore, his voice would have been amplified by other members in the coalition or association, making clear that his concerns were not just those of an isolated individual.
At this year’s CAPC Seminar, representatives from California, Colorado, and South Carolina described state-level initiatives to promote palliative care – all of which included some level of involvement from a state palliative care coalition or association. Themes that emerged from this session included that these coalitions and associations were able to:
- Establish consistent standards for palliative care
- Provide clear messaging on priority topics
- Serve as neutral sources of information (particularly critical in this time of political fragmentation)
- Facilitate and improve relationships with key stakeholders who appreciate working with a unified entity
- Develop expert technical assistance to support the implementation of a law, regulation, or other initiative
- Maintain momentum through constant (gentle) pressure when progress appears to slow
- Identify and leverage state and national resources
- Create a positive environment for new palliative care legislation and programs through the implementation of non-policy initiatives such as education and awareness campaigns
This is by no means an exhaustive list of what state palliative care coalitions and associations can do, and it is not intended to imply that all will be successful. However, it does illustrate that these entities can be incredibly powerful when harnessed effectively.
Tips for Getting Involved
Before you do anything, it is imperative that you research what palliative care organizations and/or initiatives already exist in your state. Almost every state has its own State Hospice/Palliative Care Organization/Association (some states have a joint organization), and nearly half of states have a legislatively-mandated Palliative Care Advisory Council or Task Force. There may also be other palliative care-related organizations in your state, such as the Coalition for Compassionate Care of California, the Palliative Care Network of Wisconsin, or the South Carolina Coalition for the Care of the Seriously Ill. It can also be helpful to look “outside the box” – Colorado’s Center for Improving Value in Health Care may not appear an obvious choice, yet it has been a leading driver of state palliative care initiatives.
Disease-specific organizations and initiatives (e.g., the American Cancer Society Cancer Action Network, state Comprehensive Cancer Control Programs), patient and caregiver advocacy organizations (e.g., National Patient Advocate Foundation), and even some state professional associations (e.g., medical, nursing, social work, chaplaincy, hospital, etc.) may have a palliative care component. Google is your best friend here – take the time to learn about these organizations, who participates, what their priorities are, and how you can get involved. Even if their agenda is not 100 percent aligned with your goals, participating can provide a better sense of your state and local environment, which will make you more effective if you decide to start something new.
Have you done all the research you can? Are you CERTAIN? If so . . .
Sometimes it will be necessary to launch a new coalition or initiative. If you decide that is the most appropriate route, the CAPC Seminar presenters have the following advice:
- Conduct a needs assessment – this should be familiar to anyone who has started or expanded a palliative care program! Questions you should be asking include:
- What is the gap you are trying to fill?
- What are the existing opportunities, barriers, and resources?
- What solution can you deliver that no one else can?
- What is your own capacity?
- Build a foundation by getting the “right” initial participants to help increase credibility, then build relationships with the wider community
- Reach out to non-traditional partners and be willing to spend time listening to legitimate concerns
- Be aware of and respect the need for local differences in an area – palliative care is going to mean different things depending on where people practice and/or reside
- Develop a mission and/or well-articulated goal(s), and proactively identify metrics for success
- Start small, gain experience, and aim for incremental success
- Leverage existing resources! (See next section.)
There is plenty of free research and guidance on how to initiate and sustain successful coalitions. Community Tool Box is an excellent place to start; the TCC Group also published a helpful guide on evidence-based indicators of coalition success. And while funding might be difficult to come by, it does exist. The presenters recommended starting by researching your state “health conversion foundation” (or “health legacy foundation”) and going from there.
CAPC and Other Palliative Care Resources to Help You Get Started
Even if your state palliative care coalition or association is able to obtain funding, please do not spend your precious resources attempting to “recreate the wheel!” There are many free palliative care resources that can provide a foundation for your work:
- CAPC’s “Messaging Palliative Care” webinar
- Serious Illness Strategies (note: these are actions that Medicaid health plans should take, and that State Departments of Health or Departments of Insurance could require of their plans)
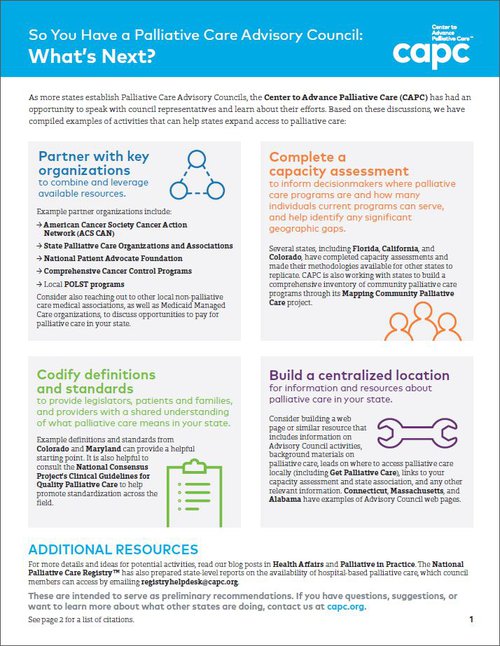
- Advisory Council One-Pager with suggestions for getting started
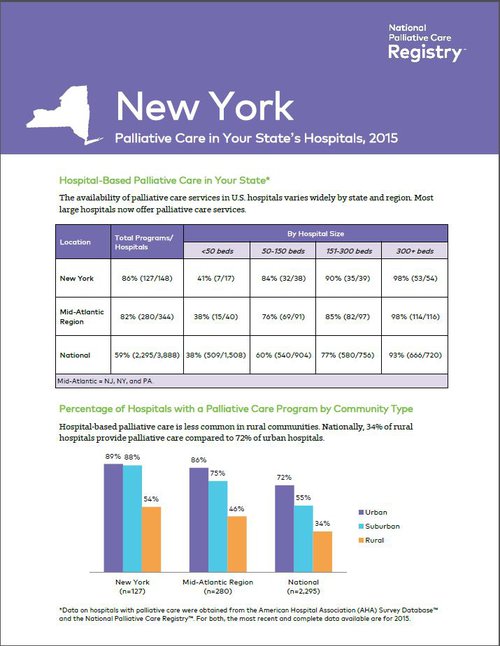
- State Reports on Hospital-based Palliative Care
- Mapping Community Palliative Care website
- GetPalliativeCare.org Provider Directory
- Palliative Care Research in the Field
- Public Opinion Research on Palliative Care (note: this includes a public-vetted definition of palliative care)
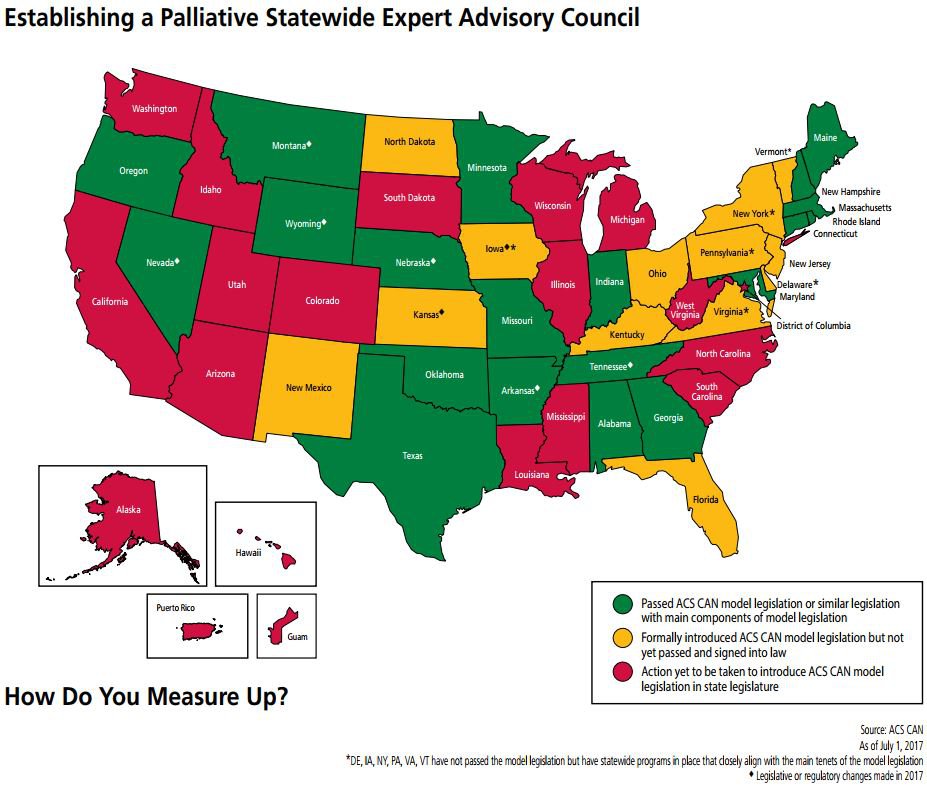
- 2015 State-by-State Palliative Care Report Card
- National Palliative Care Registry™
- National Consensus Project for Quality Palliative Care (associated blog)
Many of these resources can be found on CAPC's Policy and Payers pages.
Do you have any experiences participating in state palliative care coalitions or associations, or additional resources that you would like to share? Please comment in the space below!
Special thanks to Teeshla Curtis, Kristin Paulson, James Mittelberger, Judy Thomas, and AAHPM for sharing their experiences, which are reflected in this blog.
-
Personal details modified to preserve anonymity.
