The National Health Care Payment Learning and Action Network
Hello, Palliative in Practice readers, and welcome to the new Health Reform Quarterly! While it has taken many months to dry our tears after saying goodbye to the incomparable Emily Warner, we are thrilled to carry on her legacy of bringing you the latest and greatest in health policy and payment. When you read on, you may notice a change in that this blog is limited to a single topic. We made this change for two reasons: 1. As health reform grows exponentially more complex with each passing day – the word entropy occasionally comes to mind – certain topics demand a deeper dive in both the content and potential implications for palliative care; and 2. The field is blessed to have a number of free news aggregation emails and listservs that can help satisfy your voracious appetite for health care policy. These include AAHPM’s Hospice and Palliative Medicine SmartBrief, NHCPO’s Hospice Action Network monthly updates, and CAPC’s very own News Bites (honorable mention goes to Dr. Meier’s Twitter Feed!). Of course, you are always welcome to avail yourself of the comments section below should you have any feelings about this change – we would love to hear from you!
And now without any further ado, we bring you a recap of the 2016 Health Care Payment Learning & Action Network’s (LAN) Spring Summit.
Introduction to the LAN
In January 2015, the U.S. Department of Health and Human Services (HHS) turned the health care payment world upside down when it announced its goal of tying 30 percent of Medicare payments to quality or value through the use of alternative payment models (APMs, more information provided below) and 85 percent of all traditional Medicare (fee-for-service or FFS) payments to quality or value by 2016. To help panicked providers and health plans meet these ambitious goals – which grow even more ambitious by 2018 when the targets increase to 50 percent and 90 percent, respectively – HHS established the2016 Health Care Payment Learning & Action Network LAN.
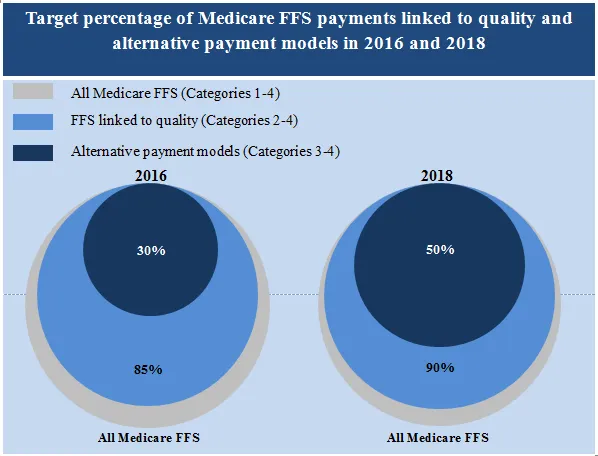
Source: CMS
Launched in March 2015, the LAN brings together some of the best minds in health care – crossing sectors and settings of care – to chart a course for how stakeholders can implement these dramatic changes. In the last year, the network has:
- established topic-specific Work Groups responsible for drafting and releasing white papers and recommendations on key policy and payment concepts
- launched a Payer Collaborative which will help inform the LAN’s approach for APM adoption
- developed three affinity groups (Consumer and Patient, Purchaser/Employer, and State Engagement) which encourage collaboration and diffusion of best practices
- convinced (through gentle peer pressure) dozens of organizations to become committed partners in setting targets for APM adoption
Primer on APMs
As the LAN started its work, it recognized early on that it needed to build consensus around just what “alternative payment models” were. So its first order of business was to create the APM Framework and Progress Tracking Work Group, which developed a framework that aligns the language of payers, providers, patient advocates, policymakers and researchers. The framework defines four categories of APMs, wherein each step up represents a move away from reliance on FFS payment.
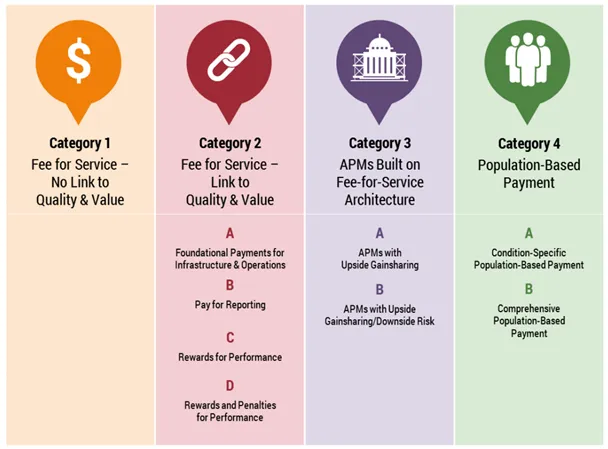
While the APM framework is chock full of excellent information (the framework above is just the tip of the beautiful figure iceberg), it’s important to highlight two overarching themes:
- Payment reform is different from delivery system reform. Implementing new payment models alone will not change health care delivery; rather, the hope is that freedom from FFS will allow providers to redesign their practice models to focus on patient needs and outcomes, instead of billable services. To quote the framework, the shift towards APMs is “necessary, though not sufficient in its own right.”
- While the framework breaks down four payment categories (nine sub-categories, if you’re picky), the end game is that most payers and policymakers are exploring one of two options:
- Payment for a defined patient population’s broad needs, or population management; or
- Payment for a defined clinical episode of health care need, or episode management.
Sure, we could confuse you by mentioning that hybrid models exist, or that payers and providers can build episodes within a population; but knowing the difference between these two approaches and thinking through how they may apply to any payment changes in your practice will put you in a better position than most.
Highlights from the Summit
While we are tempted to share with you all the excellent information we gleaned from dozens of sessions we attended, self-restraint dictates that we limit ourselves to the highlights:
The Medicare Access and CHIP Reauthorization Act (MACRA)
The impending release of the MACRA regulations provided a backdrop for much of the summit. Dutiful readers of Health Reform Quarterly may note that we have already covered MACRA once or twice before. Yet we’d like to take this opportunity to say again that MACRA IS A BIG DEAL. Remember those payment goals from HHS? This law thrusts their implementation into warp speed. While payment adjustments for MACRA won’t go into effect until 2019, the first reporting year is 2017 – yes, eight months away. And wouldn’t you know, just one day after the summit, CMS issued a notice of proposed rulemaking, aka “Everything You Wanted to Know About MACRA, But Were Too Afraid to Ask”. At a mere 962 pages, it is a first attempt to clarify issues such as which clinicians will be on the hook, what quality measures will be available and how payment adjustments will be calculated. The majority of providers will start by participating in the Merit-based Incentive Payment System (MIPS), which maintains FFS but adjusts payments based on providers’ composite quality score. However, for those brave souls who jump into the world of risk with both feet through “Advanced APMs”, the payoff could be “yuuuuuuuuge”. Expect to see summaries of these proposed regulations popping up like daisies in the days and weeks to come.
Patient Attribution and Financial Benchmarking
A critical element of APM adoption is knowing which patients you will be responsible for, and how your performance in caring for those patients will be compared to others. To help make sense of these issues, the LAN released two white papers on Patient Attribution and Financial Benchmarking. Without getting too far into the weeds, the issue of attribution in particular is incredibly important for palliative care providers. As we care for the highest-risk, highest-cost patients in the health care system, it is critical to know: 1. Whether we are being held accountable for the total cost of their care; and 2. If so, whether our performance is being compared to physicians in similar specialties or not (think comparing apples to European white truffles). While CMS is not obligated to implement LAN recommendations, expect these white papers to factor heavily into future decision-making. Therefore, we urge you peruse these documents during your MACRA reading breaks.
Chronic Care Episodes
In many ways, the LAN Summit was a celebration of the rapid adoption of APMs, which now account for approximately 30 percent of Medicare payments, and an even higher percentage of payments from many private insurers. This growth is being driven in no small part by the development of episode payments (aka “bundled payments”); therefore, it makes sense that the LAN established a Clinical Episodes Payment (CEP) Work Group early on to build a framework to tackle these complex models.
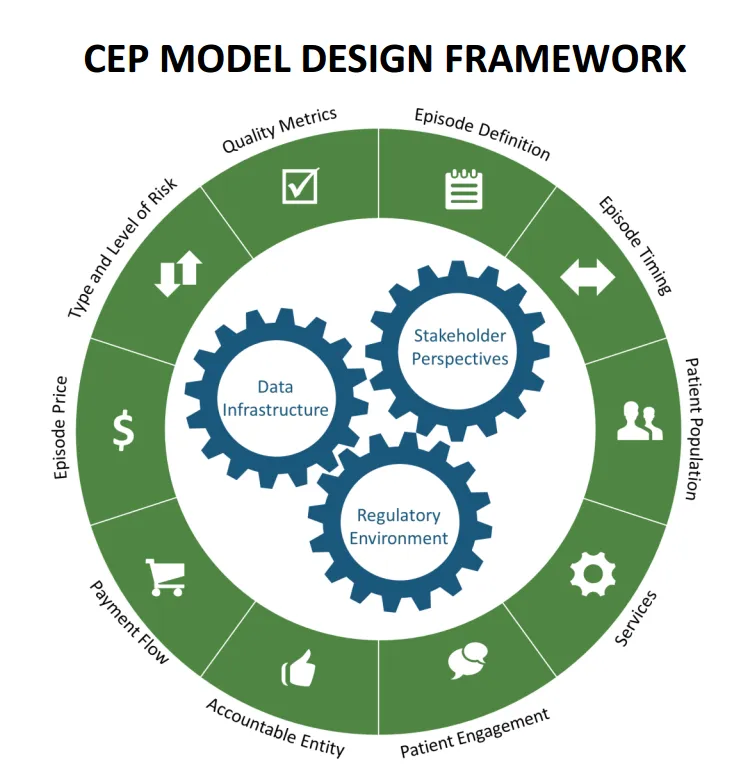
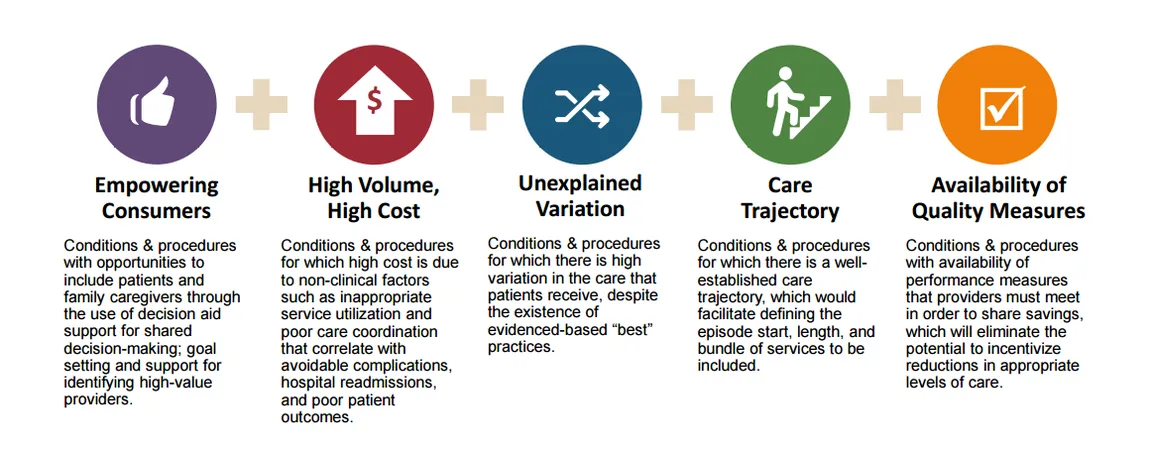
To stretch this framework’s metaphorical legs, the CEP Work Group selected three episodes in which to draft recommendations: Joint Replacement (comment period closed), Maternity Care (comment period open), and Cardiac Care (coming soon). The group started with Joint Replacement, as these episodes typically have a defined trigger point, available care pathways, and a slightly less complex population; however, members are now working on a model for Coronary Artery Disease which should be sufficiently difficult. For future opportunities, we were pleased to see that the Work Group created a selection rubric to identify new conditions and procedures that places “Empowering Consumers” at the forefront, through shared decision-making, goal-setting, and support for finding high-value providers. Hold on to your hats, palliative care providers, this could involve you!
Episode Selection Criteria
Incidentally, there continues to be growing interest in incorporating palliative care into episode management outside of the LAN as well. For instance, participants in CMMI’s Oncology Care Model are learning that meaningful goals of care discussions coupled with expert pain and symptom management can not only benefit their patients but improve their performance and bonus opportunities.
Quality and Measuring Outcomes
Last, but not least, almost all of the LAN presentations stressed the need for alignment around a reasonable number of quality measures, with several speakers favoring the use of patient-centered outcomes measures. We probably owe you a separate blog post on the palliative care quality measurement landscape, but suffice it to say, there remains an opportunity for the field here. Throughout the conference, we heard tantalizing talk of performance measures that include “reduction in pain” or “number of symptom-free days.” Of course, there remains great variability in the number and type of performance measures available; further, the desire for alignment is different than the ability to achieve consensus on a limited set of measures. Nonetheless, the continuous dialogue on patient-centered measures, particularly in pain and symptom management, could lend itself to an increasing interest in what palliative care can bring to the table.
Conclusion
In March 2016, CMS announced that it had achieved HHS’s target of tying 30 percent of Medicare payments to APMs almost a year ahead of schedule, in large part due to the efforts of the LAN. As the health care system speeds towards payment for value and the eventual elimination of FFS, the LAN will continue to be a critical thought leader. As such, all providers and payers should avail themselves of the many resources it provides (did we mention the white papers? Seriously, you should check them out). There are also countless opportunities to get involved.
Unsurprisingly, we thought the LAN Summit highlighted several significant possibilities for palliative care. The best part is that the palliative care model doesn’t need to change in order to help providers and payers meet their goals; we just need to be proactive about pursuing opportunities to partner with entities that are managing populations and/or episodes. We must continue making the case that palliative care can help deliver shared decision-making, improved outcomes, and more appropriate utilization. Coming off the LAN Summit, it seems apparent that value-based payment is here to stay. The work to be done now is demonstrating that incorporating palliative care into payment and delivery system reform will be in patients’—and the American health care system’s—best interests.

