Palliative Care’s Value in Value-Based Payment
We know that many of our dear Health Reform Quarterly readers are wondering if anything at all is happening in policy this Fall. This general election is turning out to have real implications for health care; revolutionary and industry-altering regulations are being finalized and palliative care recently took Congress by storm in a riveting subcommittee hearing on PCHETA (HR 3119) (h/t to Dr. Sean Morrison and the Patient Quality of Life Coalition!). But keep in mind: the shift from volume-based fee-for-service payment to value-based pay-for-performance is an ongoing state of affairs which – as CAPC has shared once or twice – has significant implications for palliative care. So we wonks went all-in with a systematic analysis of the roughly 10,000 federal quality reporting programs, accreditations and demonstrations, by setting, to highlight where palliative care could fit in. Enjoy!
What is Medicare Doing to Advance Value-Based Payment?
Fueled by the Affordable Care Act and a stated goal to shift at least 85 percent of Medicare payments away from fee-for-service to value by the end of 2016, the Centers for Medicare and Medicaid Services (CMS) has been rapidly implementing a variety of quality and cost evaluation mechanisms that impact provider payments. Quality and cost-effectiveness measures turn up in almost every care setting – in fact, we counted a whopping 26 current value-based payment arrangements across nine types of Medicare-serving organizations. And value will become even more embedded under the Medicare Access and CHIP Reauthorization Act (MACRA), where Medicare providers will be subject to either payment bonuses or penalties based on their performance relatives to their peers (see the National Coalition for Hospice and Palliative Care’s MACRA webinar and slides for more information).
In addition to clinician payment modifications, Medicare has implemented value-based payment programs for hospitals, home health agencies, skilled nursing facilities, hospices, and dialysis centers, as well as for every initiative out of the Center for Medicare and Medicaid Innovation (CMMI). These include accountable care organizations, oncology care models, and mandatory bundled payment programs such as the Comprehensive Joint Replacement model. (For those interested, be sure to check out the Alternative Payment Model poster featured at the 2016 CAPC National Seminar). In all these cases, provider payment can be adjusted based on performance on specified process and outcome measures. Even payments to Medicare Advantage plans can be increased based on quality performance.
What Do All of These Value-Based Payment Arrangements Have in Common?
While the specific measures used in each initiative vary somewhat, there are four palliative care-relevant “themes” found in most value-based payment arrangements:
- Patient Experience of Care measures look at patients’ overall satisfaction with their care, including how often and well their clinicians communicated with them, and how they would rate certain aspects of their care (e.g., pain relief). This is primarily assessed using some adaptation of the Consumer Assessment of Healthcare Providers & Systems (CAHPS) Survey.
- Resource use measures look at cost-effectiveness of care, including utilization and cost of care delivery. Measures in this category usually include hospital days, hospital readmissions, emergency department utilization and calculations of total spending per beneficiary.
- Care coordination measures look at processes that can allow for greater continuity of care, such as appropriate medication documentation and reconciliation, and medical record sharing and reconciliation between treating clinicians and entities.
- Assessment measures look at processes that ensure the provider is screening for and addressing issues typically occurring in their population. Assessment measures in value-based purchasing often include depression and pain screenings, as well as documentation of follow-up care plans.
Beyond the financial bonuses and/or penalties, most Medicare-serving organizations are also subject to public reporting of their performance, in comparison to their peers and competitors. While perhaps not yet as popular with the public as other crowd-sourced review sites, Medicare “Compare” sites are becoming increasingly important in this era of health care consumerism. Consider that Consumer Reports links to the Medicare Advantage quality rating each year, highlighting good, mediocre and poor performers. Thus, if the payment incentive wasn’t strong enough to strive for the best performance, there is also a powerful drive to protect the organization’s reputation. In short, these value-based measures mean a great deal to organizations and providers serving the Medicare population.
Why is this Relevant to the Palliative Care Field?
Palliative care is to value-based programs as Alicia Keys is to televised singing competitions – classy and elevates the quality of the whole enterprise. Studies and effectiveness reviews continue to show that the involvement of palliative care can improve patient and family satisfaction and experience of care; reduce days in the hospital; reduce 30-day re-admissions; reduce emergency department visits; and, especially towards the end-of-life, reduce total spending. This means that increasing the involvement of palliative care can improve value-based performance in hospitals, home health agencies, skilled nursing facilities, dialysis centers, accountable care organizations, oncology care models, bundled payment programs, and Medicare Advantage plans.
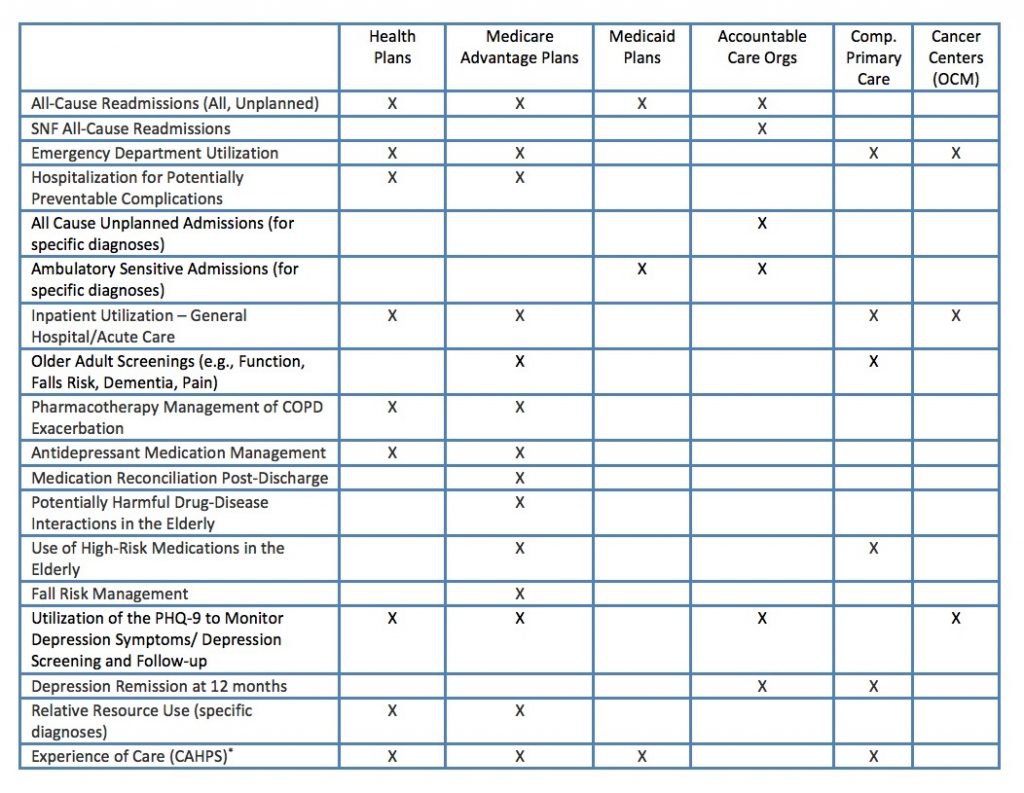
The table below highlights some key performance measures across key entities, and shows where the literature suggests that palliative care can improve performance:
In sum, our colleagues across the health care system are being evaluated – and paid – on measures that palliative care can impact. So get your elevator speech ready and let’s use this opportunity to bring “palliative care everywhere!”
And with that, we’ll sign off for now – but keep your eyes peeled for communication from CAPC about the MACRA final rule. We’ll see you in 2017!


