Finally, Proof that Palliative Care Improves Outcomes for Patients with Advanced Heart Failure
A Review of Palliative Care in Heart Failure: The PAL-HF Randomized, Controlled Clinical Trial by Rogers et al.
What Did They Find?
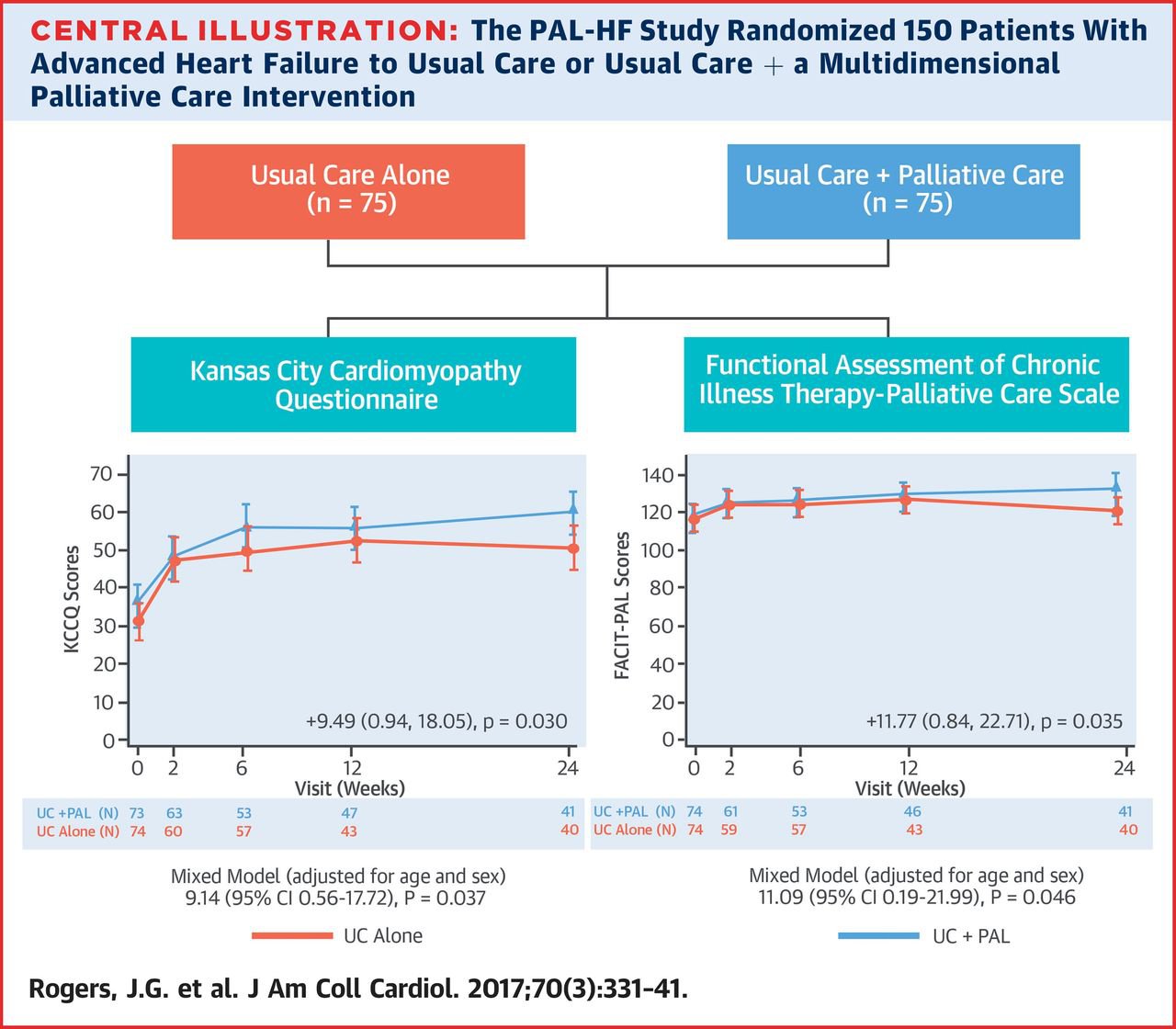
In their randomized controlled trial evaluating the benefits of palliative care for patients with advanced heart failure, Rogers and colleagues have shown that patients who received palliative care had better outcomes for quality of life, anxiety, depression, and spiritual well-being when compared to patients who did not receive palliative care. The diagram below illustrates the key findings—that the intervention improves scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ) and the Functional Assessment of Chronic Illness Therapy—Palliative Scale (FACIT-PAL). These tools are standard scales used to measure quality of life in patients with heart failure, and in palliative care populations, respectively.
What Did They Do?
Their single-site study randomized 150 patients to usual care vs. palliative care + usual care and followed the patients for six months. The palliative care intervention consisted of a palliative care-trained nurse practitioner and physician dyad that followed patients while in the hospital; the palliative care nurse practitioner then actively followed patients in the outpatient setting. Physical symptoms, advance care planning, psychological, social, and spiritual domains were all assessed and addressed.
Commentary
This clinical trial, which was funded by the National Institutes of Health, is one of the first well-conducted randomized trials to evaluate the role of palliative care for patients with advanced heart failure. The authors were clear from the outset that demonstrating palliative care impact on quality of life, not survival or changes in utilization (e.g., reduction in hospitalization or emergency room visits), was their primary goal. To understand why this was the case, consider the different trajectories of heart failure and cancer—the disease in which most palliative care trials have demonstrated improvements in utilization. Admissions for patients with cancer are often related to uncontrolled symptoms (which can be avoided through good palliative care and oral medications for outpatients). For patients with advanced heart failure, hospital admissions are often the result of disease exacerbation that needs to be treated with medications like intravenous Lasix or inotropes—medications which, in most health systems, can only be provided in the hospital setting.
While it may at first glance be disappointing that this trial did not find a survival advantage, such as that found by Temel and colleagues in their landmark New England Journal of Medicine study of patients with cancer, this trial has significant implications for patients with advanced heart failure. Indeed, as the authors point out, while the trial may not demonstrate that palliative care makes people live longer, it shows without a doubt that patients live better—an outcome that matters to patients and their families.
There are some limitations that must be considered when interpreting this study. It was a single-site study at an academic medical center where palliative care is already well-accepted and integrated into the culture of the hospital. The study excluded patients who were thought to be candidates for ventricular assist devices (VADs) or heart transplant within the next six months. In 2013 CMS mandated that all patients who are candidates for destination VADs see palliative care specialists; the data from this study may or may not be replicable for these VAD candidates whom palliative care is asked to consult.
Despite these limitations, this article is a bold and important step forward in integrating palliative care into the care of patients with advanced heart failure. Of note, this trial was particularly ethnically diverse—more than one-third of patients in both groups identified themselves as African American. This suggests that the results are generalizable across ethnic groups, thus strengthening the applicability of the results to many different populations and settings.
Clinical Bottom Line
For patients with advanced heart failure, palliative care has a clear benefit in terms of quality of life, anxiety, depression, and spiritual well-being. This article can be used to improve integration with cardiologists, as it demonstrates that palliative care helps patients with advanced heart failure live better while they undergo efforts to prolong their lives.
For patients with advanced heart failure, palliative care has a clear benefit in terms of quality of life, anxiety, depression, and spiritual well-being.
Don't forget to take CAPC’s case-based course, Relief of Suffering Across the Disease Trajectory: Heart Failure, and earn CE credits and MOC points (ABIM).
