Eyes on the Prize Part II: Palliative Care Post-Election
The song Eyes on the Prize was adapted in the 1950s from an old spiritual. The lyrics are about persevering despite obstacles, a theme as relevant as it has always been to the future of palliative care and the people we serve:
As is true with any change of Administration, this is a time of uncertainty, and so it’s worth evaluating the likely future of the palliative care field—as we continue to try to improve the care received by people with serious illnesses.
Bottom line: we think the foundations of our field and the reasons for our work are not only unchanged, but heightened, as a result of the 2016 Presidential election. The field of palliative care has grown rapidly in the past 10 years, responding to many developments. These include:
- the growth in number and complexity of persons with chronic disease;
- the success of modern medicine at converting once rapidly-fatal illnesses (like cancer and heart failure) into chronic conditions with which people often live for many years; and
- the expanding body of research demonstrating the impact of palliative care models on the triple aim (better quality of care, quality of life, and cost-efficiency) in the care of this high-need, high-cost population.
Abundant evidence of the impact of palliative care on patient and family wellbeing as well as avoidance of preventable hospitalizations, ICU stays, procedures, and burdensome transitions has increased the rate of integration of palliative care in the U.S. The adoption has been most obvious in hospitals, but is now also spreading to cancer centers and other specialty practices, nursing homes, and home care.
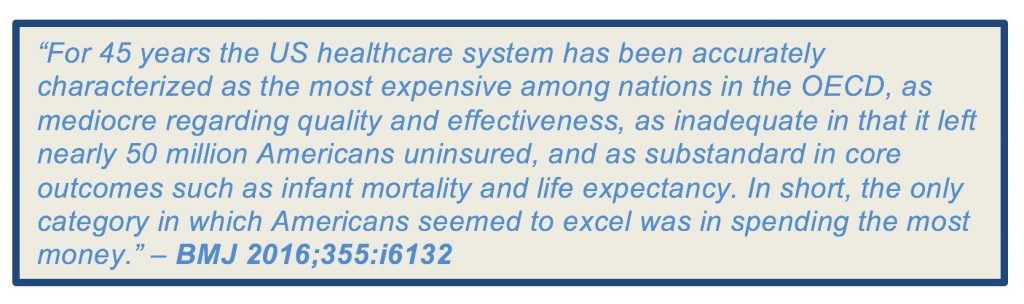
If health care spending continues its current rate of rise, a decade from now, the majority of all mandatory federal spending will be for Medicare, Medicaid, and Social Security. This leaves ever-decreasing amounts of the federal budget for discretionary spending on education, transportation, food and drug safety, infrastructure, and the military. Because this situation is neither sustainable nor desirable, and because fundamental reductions in the rate of growth in health care spending are required regardless of which party is in power, the focus of health policy in past decades has been on improving value, or increasing the benefits resulting from medical care per dollar spent.
The ACA attempted to improve access to care via the Exchanges and Medicaid expansion, to ensure that when individuals buy insurance they get reliable coverage that covers essential benefits, and to pay for this coverage expansion by taxing devices and high benefit (Cadillac) health insurance plans, while decreasing Medicare spending through a range of new delivery and payment models.
Among the many innovations claiming to improve value since passage of the ACA, few have a stronger and more consistent track record of actually doing so than palliative care, delivered through a range of models and settings. And since our patient population accounts for more than half of all healthcare spending, demand for this service model isn’t going away.
Despite these economic and demographic realities, the recent election has resulted in uncertainty about whether our government and health system will remain committed to improving value. Some chaos and uncertainty is likely—nothing new for those of us who work in palliative care—but there is reason for confidence about the importance of value and the role of palliative care going forward. It is likely that pressure to improve value—strengthen quality and reduce costs—will only accelerate in coming years. Why do we believe this?
- “If you break it, you own it.” In a rush to dismantle the ACA, and Medicaid, and Medicare, the party in power faces political risk including losses in the mid-term elections, and rage from the base when health care becomes both more expensive and harder to access. Because of this, it is arguably likely that little impact of repeal will be felt until after the 2018 mid-terms, and that the main immediate effect then may be elimination of the Medicaid expansions, which will also have major negative consequences for politicians at all levels of government. Support for care models that help seriously ill people remain stable in their communities and able to avoid crisis ED and hospital visits could help mitigate these political consequences.
- States need relief: The cost that our current broken heath care system imposes on society is only worsening with the aging of the baby boomers (10,000 of us turning 65 each day). The economic consequences multiply as informal caregivers lose productive work and become chronically ill themselves. All this puts enormous strain on state budgets. The impact of palliative care teams and principles (working in partnership with our colleagues across the continuum) on rational delivery of health care that matches the needs and priorities of patients and those who love them is more relevant and important than ever.
- Shifting Risk: We agree with many of the pundits arguing that a key strategy will be continued shifting of risk away from government and payers to providers and patients and families. Health care organizations and clinicians will be expected to take on more downside risk, and patients and families will have ever narrowing networks, while their deductibles, co-pays and insurance costs continue to rise. This shift in risk will be accelerated by the rise in uncompensated care (yet more risk falling on providers and patients) if the Medicaid expansion is rolled back. More “skin in the game” increases demand from consumers (patients and families) for meaningful shared decision making and high value care. Demand to avoid preventable and costly (especially hospital and pharmaceutical) services will only grow, driving demand for palliative care for the seriously ill. Stronger movement toward value for all parties opens up avenues to pay for palliative care services. Our work is vital to their success and survival.
Specifically, community-based palliative care aligns with patient preferences (cost effective care), with payer strategies (better management of high risk patients), and health system needs (more reliable system of care, capable of success within a risk contract). And inpatient palliative care has a critical role in identifying high risk patients and helping to ensure that their trajectory of care (in and out) is appropriate and aligned with patient and family preferences, as well as ensuring reliable communication and handoffs between inpatient and community services.
- Medicare Advantage: Medicare is the proverbial political third rail, and risky for the new government to threaten through “vouchers.” What seems probable instead is more privatization of Medicare, with a lower bar for entry into the Medicare Advantage (MA) market by insurers, fewer federal regulations for those MA plans, and higher co-pays and deductibles in traditional Medicare. This change will drive beneficiaries out of regular Medicare and into the MA private sector. Medicare Advantage plans right now are leading the healthcare industry in investment in palliative care-type benefit designs (e.g., Aetna, Regence Blue Cross/Blue Shield, HCSC), use of palliative care vendors (Aspire, Turn-Key, Landmark), and attention to the social determinants driving much of health care utilization.
- Managed Medicaid: Assuming Medicaid moves to block grants, States and organizations that serve Medicaid patients and uninsured people will of necessity focus on high value care and incentivize community–as opposed to hospital–and institutional long term care – models. Growth in home and office-based palliative care-like models with increasing reliance on whole-person care (including community health workers) for the seriously ill could result.
- MACRA+CMMI: Among the few strongly bipartisan pieces of legislation in the past 8 years, MACRA replaces the Sustainable Growth Rate in an effort to rein in provider reimbursement, with a gradually rising imposition on clinicians of payment for value, not volume. MACRA is completely independent of the ACA and is not included in “repeal and replace.” Over time under MACRA, clinicians will either demonstrate improved quality and constrained spending or see their reimbursement fall. Because MACRA’s success depends critically on the support and infrastructure enabled by the Center for Medicare and Medicaid Innovation (CMMI), the likelihood of CMMI survival increases. CMMI may also be difficult to eliminate since the Congressional Budget Office currently estimates that CMMI’s activities will reduce federal spending by $34 billion from 2017 through 2026. There is also strong support from some powerful forces in the health care industry to continue the drive towards value-based care. Palliative care knowledge and skill are essential to clinician success in terms of improving both their quality and resource utilization under MACRA (or CMMI’s advanced alternative payment models). This can give our field a “safe harbor” in which to move forward.
Think of it like a family meeting
Our role in the broader health system and the organizations we work for now is comparable to our role when we lead a family meeting. There are different belief systems and cultures in conflict. There is uncertainty— in an already chaotic environment—that may inhibit willingness to make decisions, future commitments and, in the case of leadership, funding tradeoffs. This uncertainty may affect timing, so we have to be patient, just as we would when reviewing difficult clinical decisions with our patients and families. And just as we offer time-limited trials of therapies to patients and families under conditions of uncertainty, a similar uncertainty may open the door to receptivity for low-risk, high-impact solutions that can be put in place now as pilots, and that will help regardless of the nuances of reform. Opportunities to expand access to palliative care may also arise from these circumstances.
Throughout, we can focus on unifying values to build forward with our fellow human beings, who are more alike than they are different on the essentials—the desire for a good quality of life, independent function, honoring strong family relationships, being at home when possible, and a sense of meaning and purpose. Our skill and ability to listen and hold conflicting emotions and realities, and to model calm in the midst of the storm, will be needed now. People with serious illness need relief from suffering and they need care that is an expression of who they are and what matters most to them. This is true regardless of changes in government. Our work of the past 20 years has resulted in markedly raised levels of demand for palliative care and awareness of the importance of these objectives.
What is to be done now?
Here’s our short list of no-regret, low-risk, actions that will both keep our eyes on the prize–focused on the main thing–and prepare us to negotiate with people who will want to pay for our services:
- Stay focused on meeting patient and family needs – ensuring their independence, good symptom management, and appropriate care. Eyes on the prize.
- Make time to accelerate relationship-building with key decision-makers who are facing the challenges of improving quality and cost of care amidst a chaotic financing and regulatory environment.
- Raise our own game – by getting better at defining and costing reliable service bundles (the old “what’s in the syringe” question), how to scale up our services quickly, and how to better use existing resources to highest impact.
- Be flexible – new opportunities will emerge – let’s be ready.
