Embedded RN-Led Clinics in Primary Care Practices
As a palliative care physician at Partners in Care, a non-profit, community-based hospice and home health agency in Bend, Oregon, it’s my goal to impact the care patients receive well before they land in the hospital in crisis. In 2014, we launched our outpatient palliative care program, and what started with me seeing palliative care patients in the oncology practice of a multi-specialty group, has now developed into a thriving outpatient practice.
In order to reach more patients further upstream in their disease trajectory, we created a nurse-led palliative care clinic embedded within primary care clinics. Our program has, so far, achieved excellent results in pain and dyspnea scores, advance care planning rates, completion of POLST, and increased hospice referrals and length of stay (LOS).
Building a Nurse-led Palliative Care Program
Our program is modeled on a nurse-led palliative care program at Providence Clinic in Everett, Washington. Our team includes three palliative care RNs, all of whom were previous hospice nurses. We were extremely fortunate to have Velda Filzen, the nurse who ran the Everett clinic program, working with us to help mentor these nurses as they got started. They initially did home visits with Velda, and she was there in clinic with them for the program start-up to help mentor, model conversations about advance care planning, and teach consultation etiquette. In addition, to get more palliative care training, the nurses spent time with me in the oncology clinic and took CAPC’s online courses. We have weekly IDT meetings and regularly review patients with active issues. We try to meet patients on the same day as their primary care provider (PCP) visit, and target specific patient populations, especially those:
- Felt to be within their last two years of life by the treating PCP
- Requiring clarification of care goals or help with advance care planning
- Requiring symptom management related to one or more serious medical illnesses
High Lakes Health Care is an independent primary care practice with three locations in Bend. Our palliative care RN covers all three sites weekdays 8:00 am-5:00 pm, though she spends the most time in the clinics where she is busiest. Mosaic Medical is a rural Federally Qualified Health Center (FQHC), 36 miles from Bend in Prineville, Oregon, and our RN sees patients there two days per week. A third nurse sees predominantly home-bound patients, the majority of whom also served on our certified home health program. Our palliative care physician is available for consults as needed for more complex patients and is always available to discuss patients with the embedded RNs as well as with the patient’s PCPs.
Next month, we will expand to another rural Mosaic clinic site two days per week, and we hope to expand our team to include a dedicated social worker and chaplain.

Financing
The embedded RN program is currently supported by our hospice, leveraging the income resulting from the larger number of referrals and the longer hospice LOS. Currently, less than a year into the program, we are losing money, though the program we are modeled after was able to offset the salaries of eight full-time palliative care nurses. If volume increases as expected, we plan to add a nurse practitioner who could bill for visits, and are also working towards RN billing for their advance care planning work. Our nurse-led program will be sustainable if we continue to increase hospice referrals and achieve longer LOS on hospice. Early results indicate steady increases in these quality metrics.
Program Data
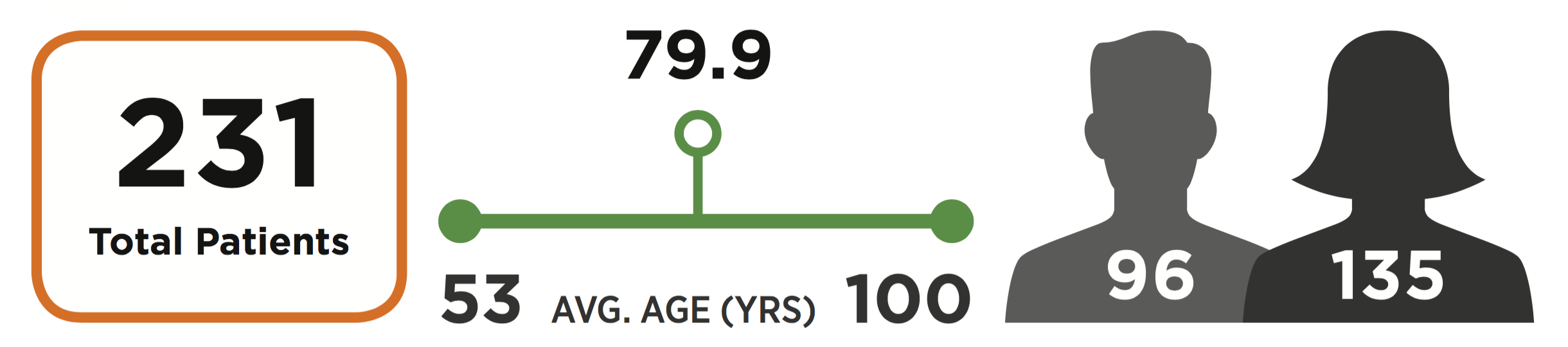
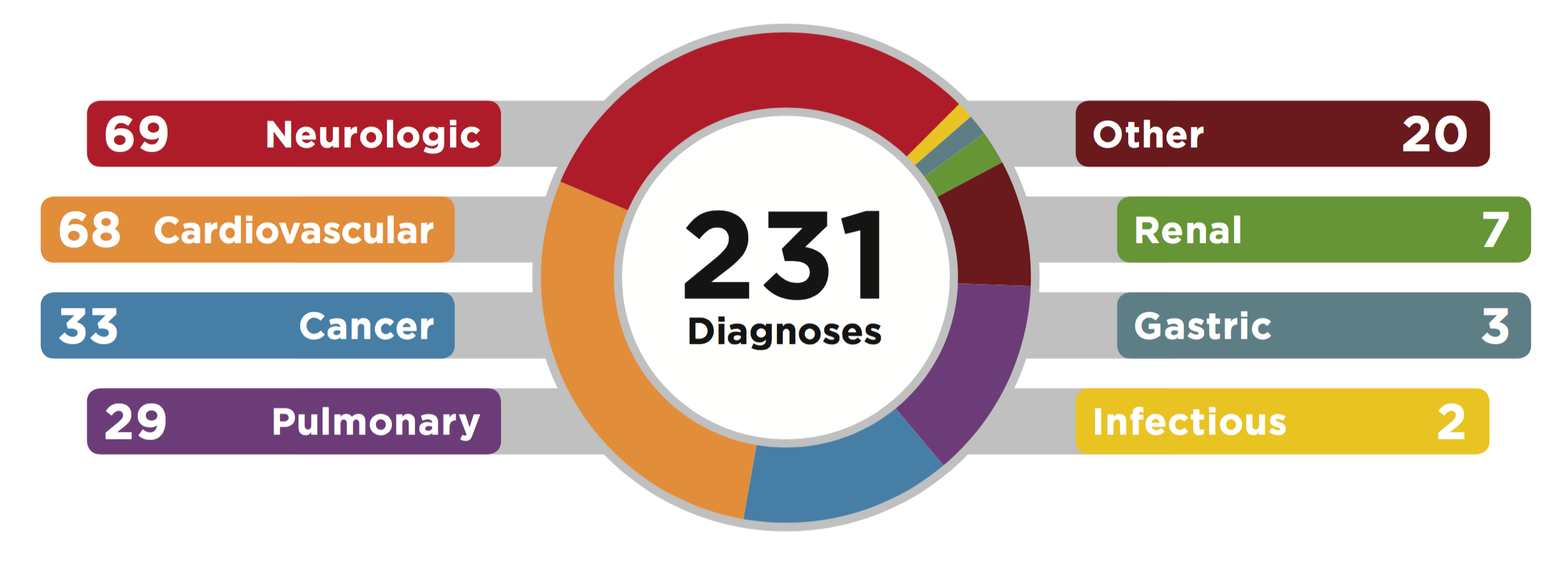
In the first 11 months of 2017, our palliative care nurses saw 231 patients with a variety of diagnoses. Face-to-face visits make up only 31% of total contacts with primary care patients; the majority of contact is by telephone, with more than 1,400 calls made in 2017. Below is a breakdown of our patient demographics and diagnoses.
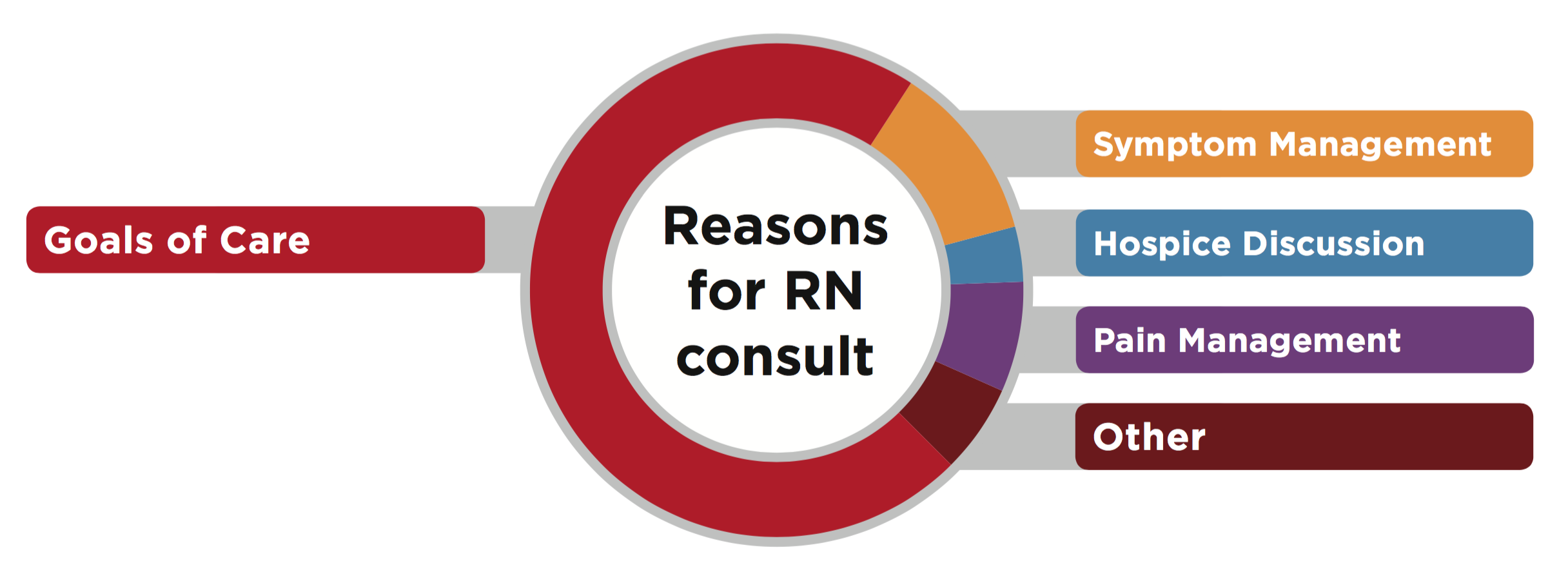
The reason for the vast majority of our visits is discussion of care goals, followed by symptom and pain management.
Our palliative care nurses discuss advance care planning with the vast majority of patients, with approximately 40% completing POLST.
Of our 231 patients, 63 were referred to hospice, with an average LOS of 60 days. Three of our patients died on our service before they could be referred to hospice.
In the three years since we embedded palliative care nurses into different models of primary care clinics, we are seeing positive results. We have increased referrals to hospice and home health, and more patients are completing advance directives and POLST. Additional benefits include increased awareness about palliative care among primary care providers. Dr. Jessica Morgan, the medical director of High Lakes Health Care, says, “I have always valued patient quality of life, especially near end of life, but have not had the resources or skills to do this well in my practice. Palliative care has given me the tools and support to provide this care for my patients.”
Primary care providers often have long-term and emotionally-invested relationships with patients that make prognostication and timely discussion of goals and priorities for care challenging. We team with PCPs to ensure patients are getting the support they need, to clarify care goals, treat symptoms aggressively to improve quality of life, and refer patients to hospice when appropriate.
As with any new program, there have been challenges. The majority of patient contact is by telephone, often after an initial face-to-face meeting while the primary care provider is seeing the patient. “Warm handoffs” improve collaboration with PCPs and increase patient comfort with palliative care, because they see us as part of their PCP’s team working closely with the providers they trust. Providers in some clinics were slow to warm to the idea—and some are more excited about our partnership than others—but in a short time we have seen incorporation of palliative care practices (routine advance care planning, symptom assessment and management) into their practices.
Conclusion
Partnering with these clinics has been invaluable, as PCPs now better understand what services are available to their seriously ill patients, and they better utilize our full continuum of both home care and hospice services. We look forward to further integration over the coming year in order to empower even more PCPs to have the support they need to provide higher quality care to their sickest patients.
Learn More
CAPC members have access to a robust online curriculum for training all frontline clinicians in core palliative care skills. All clinical courses offer free continuing education credits for physicians, physician assistants, nurses, social workers, case managers, and licensed professional counselors. Find out if your organization is already a CAPC member, or learn more at capc.org.
